TRANSFORAMINAL ENDOSCOPIC DISCECTOMY AND
FORAMINOPLASTY
“An experience since 2000 and of over 1800 cases”
Eric GOZLAN (PARIS, France) - IITS PHOENIX, May 2009
PURPOSE:
The author discusses his experience of treating lumbar disc herniations and foraminal stenosis by Transforaminal Endoscopic Discectomy (TED).
SUMMARY OF BACKGROUND DATA
The experience started with the publication in 2002 of the 50 first cases in France of disc herniations treated by TED, with 90% positive results and less than 1% complications.
The main study, which exposed the complete technique and indications, was published in 2003 and related to 114 cases with similar results at 3 and 12 months.
In 2005, a multicentric study was carried out concerning 644 patients treated with the same technique. The results showed an 83.4% success rate at 3 months depending on the learning curve and 1.08% complications.
Another study was published in 2007 about TED after FBSS (125 cases) with 87% success rate and still no major complications.
The last study (2007) concerned foraminoplasty in lumbar degenerative foraminal stenosis, regarding 201 patients with a success rate of 89% at one year post surgery.
INITIAL EVALUATION:
From January 2002 to January 2007, 1223 patients were admitted in this study and evaluated at 0, 1 and 3 months (1223 cases) and 12 months (688 cases)
Sex ratio was M/F = 1.037, mean age was 46.2 years (min=16, max=86).
Average duration of symptoms was 3.2 years for recurrent cases and 9.9 months for consecutive evolutionary cases.
357 patients (29%) presented neurological signs.
236 patients (19.3%)had already had primary surgery and 45 chemonucleolysis (3.7%).
Also, Foraminoplasty had been performed in 316cases (26%).
RESULTS:
- At 3 months post operatively we noted that:
Neurological signs had disappeared in 88% of the cases.
Radicular pain was reduced on average by 81% on the AVS and lumbar pain by 65%
The DALLAS score was reduced by 53%
Also, 87% of the patients considered the result as a success.
- At 12 months post operatively (688 patients) the results were:
Radicular pain decreased on average by 88% and 74% for lumbar pain.
The DALLAS score reduced on average by 63%.
The success rate increased to 91%.
The rate of complications was very low (1.06%), as in the other studies.
DISCUSSION:
It becomes actually evident that the goal of spinal surgery is to require, more than ever, the least amount of iatrogenic effects.
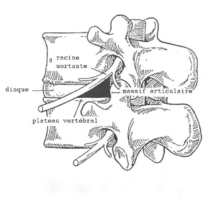
The transforaminal approach brings the best answer, by avoiding transcanal effraction with a limited annular fenestration, a minimal access to the epidural space and above all without destabilization of the intervertebral joint.
By acquiring experience, the author has enlarged his indications by treating intracanal, foraminal, extraforaminal and extruded herniations as well as lateral stenosis.
He especially underlines the importance of the provocative discography to confirm the symptomatic discs and to evaluate the extension of annular tears.
In his opinion, one of the best successes of this technique is to be able to treat efficiently patients with failed primary open surgery.
This minimally invasive technique also allows it to be repeated in case of failure or recurrence, with a similar rate of success and complications.
CONCLUSION:
Endoscopic spinal surgery has now reached its maturity, appearing as a real functional method as well as did arthroscopy and coeliosurgery a few decades ago.
The author’s experience suggests that this endoscopic microsurgical technique on the spine is an extremely efficient and safe method, to the patient’s benefit.